“It shouldn’t be just the mother’s issue”: Fathers’ involvement in lactation practices and care following infant death
MONDAY, AUGUST 30, 2021
In the lead up to Father’s Day we bring you this heartfelt article written by Dr Debbie Noble-Carr and Dr Katherine Carroll from the Australian National University reporting on their study of lactation after infant death.
The article highlights the value Dads in the NICU place on infant feeding and breastmilk, and the part they can play in supporting their partner with lactation practices and care, but also emphasises how, following the unbearable experience of infant death, fathers remain aware of their partner’s lactation needs and their desire to support them continues (including through breastmilk donation).
Quotes from study participants are included, with pseudonyms provided to protect anonymity. If you require support please reach out to any of the organisations listed at the end of the article.
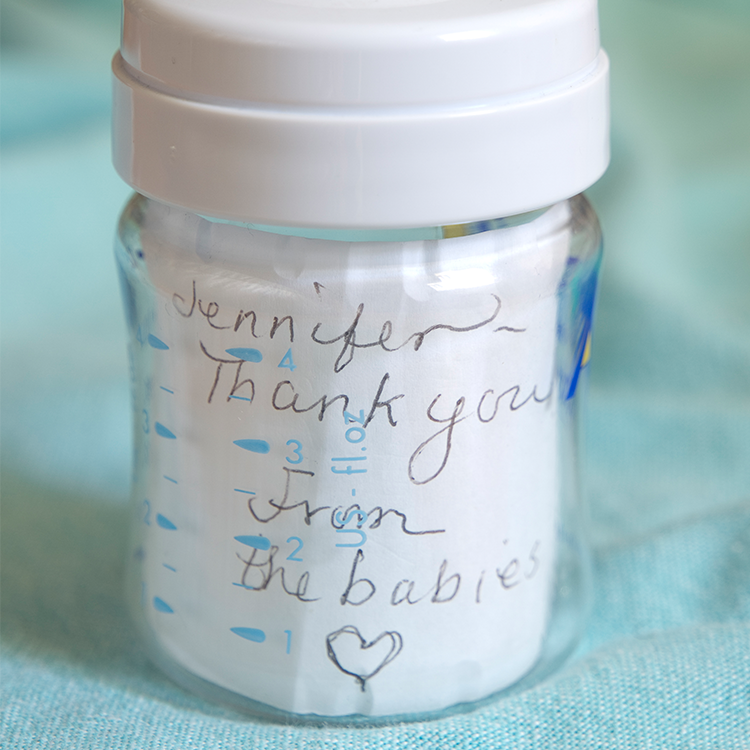 Image source Mark Manger
Image source Mark Manger
Infant feeding can be a challenging, but deeply meaningful experience for both mothers and their partners whilst their infant is in the NICU. In a study being conducted by the ANU, fathers told researchers they appreciated support from health professionals to be directly involved in lactation and infant feeding prior to and following the birth of their baby. Fathers explained that infant feeding practices enabled them to develop a deeper bond with their baby and provided a way for them to perform important parenting roles:
“It was really special when we were able to first feed our baby Sarah’s milk, we were brought into that process as well, and the nurses let me squeeze the syringe! Like feed our baby. That, to me, was more important than being able to help change his nappy, or change his sheets” (Matt)
Fathers were often primary and significant supporters to their partners within NICU settings, and as such, they also appreciated being informed and included in conversations about breast care and requirements for breastmilk expression. Fathers acknowledged that keeping up adequate supplies of breastmilk was often challenging for their partners, and they wanted to be informed so they could provide them with appropriate practical and emotional support. For some fathers this involved ‘hands-on’ assistance with breastmilk expression:
“It seemed to be a lot of work just to get a couple of drips of colostrum out to suck up in a syringe…she had quite a lot of trouble, I suppose, just massaging for half an hour and all that, so I’d help her with that. To massage the breast and get them flowing. Eventually I think whatever, I must have spent a bit of time there in that week...I got pretty good at it, at massaging and getting the flow” (Andrew)
Tragically, not all NICU babies survive. And although it is often not recognised or discussed, in the wake of infant death, the need for lactation care and support often remains. Following stillbirth or infant death, mothers are often faced with the complex task of managing the initial onset or continuation of their lactation. Families may also be left with frozen stores of breastmilk in the hospital or in the home.
Despite the challenging, confronting and confusing nature of lactation in this context, bereaved mothers typically receive little support from health professionals to make informed decisions about how to manage their lactation or existing frozen stores of breastmilk (Noble-Carr et al., 2021). As a result, many fathers also remain unaware of their partner’s bereaved lactation care needs and feel unsure of how to best support them.
However, a recent report released by the ANU (Carroll et al., 2021) found that some fathers, especially those who witnessed their partner expressing breastmilk after infant death, were intimately aware of their partner’s lactation. These fathers actively sought ways to better support their partner to manage issues such as breast engorgement or milk leakage and the subsequent emotions these experiences elicited for them.
“I remember being in the hospital still that afternoon, after our baby passed away, and Sarah was just like, ‘My boobs are going to explode. What do I do? What do I do?’ And the nurse just sort of rolled in a pump and was just like, ‘use the pump’....It was like a really clear moment, just looking at this milk, and it was like, it was the one thing she could do for our baby and now she was just like ‘What do I do with this? Do I pour it down the sink?’”(Matt)
Matt and his partner were one of seven couples in the ANU study that made the decision to donate their breastmilk to a Human Milk Bank (HMB) following their infant’s death. Fathers were often involved in making the decision to donate milk. The emotional and practical support they provided to their partner was integral to either one-off donations of frozen milk or ongoing donations from mothers sustaining their expression. Some mothers continued breastmilk expression for many months following the death of their baby, and consequently donated many litres of milk to HMBs.
Fathers said that providing support to facilitate their partner’s donation, especially donation from sustained breastmilk expression, was demanding and challenging. Chris, one of the fathers in the study, explained what this support involved:
“Supporting her and being up with her in the night, caring for her and making things easier for her, and making sure that she didn’t have extra labour of having to wash bottles and sterilise the pump, and all this sort of stuff” (Chris)
The magnitude of this support is best understood, when acknowledging it co-existed with fathers' attempts to come to terms with their own grief and in many cases the need for them to take full responsibility for the general running of the household, care of children and returning to work. Although demanding, fathers overwhelmingly said bereaved donation was worth all the work. Fathers expressed enormous pride in their partner’s breastmilk donation and explained the shared process and act of bereaved donation was beneficial to both of them.
“The act of expressing and donating the milk took the focus away from Maria and her pain, and put it on something else, so she had a purpose and another focus, and there was a reason to express because she could donate it to other babies, and she could help all these other babies…As a purpose for her, there was a purpose for me as well, and yeah, I did find a lot of significance from doing that, and it was a shared duty, I guess, that we took on together to do this. We did it together” (Chris)
All of the fathers involved in bereaved breastmilk donation explained that helping others and having something positive result from their devastating loss had helped them in their grief:
“It was an opportunity to donate the milk to help other people keeping them alive and basically keeping a memorial to our baby at the same time” (Sebastien)
The ANU study is the first in the world to talk to bereaved fathers to determine that bereaved milk donation can be deeply meaningful and beneficial to not only mothers, but also their partners. Not surprisingly, all bereaved fathers participating in the ANU study suggested that donation should be an option that is more readily available to bereaved families across Australia.
Regardless of whether families want to, or can donate breastmilk following loss, fathers in the ANU Study stressed the need for health professionals to acknowledge that they too may attach meaning to breastmilk and lactation practices following their infant’s death and they need to be provided with appropriate information to enable them to better support their partners with bereaved lactation care.
As we approach Father’s Day we would like to acknowledge these fathers’ experiences and thank them for their courage and generosity in sharing their collective wisdom. We acknowledge that partners of birthing parents who do not identify as men or as fathers may also share similar experiences and that their unique needs should also be included in future research and considered by health professionals.
If you’re a Miracle dad and you are needing extra support, you can find help with the following links:
Miracle Babies Foundation NurtureLine on 1300 622 243.
Red Nose (including SANDS): www.rednosegriefandloss.org.au or 1300 308 307
Australian Breastfeeding Association or 1800 686 268
References:
Noble-Carr, D., Carroll, K., & Waldby, C. (2021). Mapping Hospital-Based Lactation Care Provided to Bereaved Mothers: A Basis for Quality Improvement, Breastfeeding Medicine, 1-11, DOI: 10.1089/bfm.2021.0089.
Carroll, K., Copland, S., Noble-Carr, D., & Waldby, C. (April 2021) Lactation After Infant Death: Partners’ Experiences – A pilot study funded by the Newborn Intensive Care Foundation. https://sociology.cass.anu.edu.au/research/publications/lactation-after-infant-death-partners-experiences).
Acknowledgements: The authors would like to acknowledge Simon Copland who conducted interviews with fathers and led the data analysis on this study. Funding was received from Australian Research Council (Discovery Grant DP180100517) and Australian National University. Particular thanks to the Newborn Intensive Care Foundation who provided funds to include bereaved fathers in the study.



